The Ultimate Guide to Colostrum Collection (Prenatal & Postnatal): How to Prepare, What You Need, & Step-by-Step Hand Expression
- drapejess
- Nov 18, 2025
- 8 min read

By Jess Draper, IBCLC, Infant & Toddler OT, Holistic Pelvic Floor Therapist | Hali’a Therapeutics – Eugene, Oregon
Collecting colostrum—often called liquid gold—is one of the most valuable ways to support your baby’s feeding, immunity, and early gut and brain health. Whether you’re collecting prenatally or expressing colostrum in the hours or days after birth, having the right guidance can make your experience smoother and more effective.
As an IBCLC, holistic infant & toddler occupational therapist, tongue-tie specialist, and pelvic floor therapist, I support hundreds of Oregon families through colostrum harvesting every year. This guide brings together the most important, evidence-based information parents need—all in one place.
This article covers:
✔ Why you should consider collecting colostrum prenatally
✔ Supplies you need
✔ How to hand express
✔ When to start prenatal colostrum harvesting
✔ Contraindications and safety
✔ How much is normal
✔ Storage, freezing, and transporting
✔ When to use pumping vs hand expression
✔ How to use colostrum after birth
✔ Troubleshooting and partner support
✔ Oregon-specific resources for local families
Let’s help you feel confident, prepared, and supported.
What Is Colostrum and Why Is It Important?
Colostrum is your first milk—thick, concentrated, nutrient-dense, and packed with immune factors your baby can’t get anywhere else. Your pregnant body starts making colostrum as early as week 12 of pregnancy! It is the first stage of milk you produce until ~3-5 days postpartum when your milk begins to transition. Research has shown that when the first food your newborn receives is colostrum, it helps to seal the gut and provide your little one with immunity against allergies, asthma, autoimmune diseases, and inflammatory bowel disease. It also reduces the likelihood of your infant developing Necrotizing Enterocolitis (NEC) - a very serious gastrointestinal disease.
Why Consider Harvesting Colostrum Prenatally?
As an infant OT + IBCLC specialized in infant tension and oral motor development, I regularly use harvested colostrum to support babies through those early hours when feeding may be trickier. Many babies benefit greatly from having previously harvested colostrum on hand at birth. There is no way to predict if your baby will have feeding challenges, need to be separated from you, or have glucose or jaundice - but in all of these scenarios having a stock of colostrum going into delivery can help prevent the need for supplementation.
Supplementing in the early days makes it incredibly hard to increase your supply to meet baby's demands for that whole first month, which causes many parents to cease breastfeeding earlier than they originally planned.
Other reasons your newborn might need colostrum :
Tongue ties
Lip ties
High palate
Body tension (torticollis, birth strain, vacuum/forceps delivery)
Prematurity
Jaundice
Sleepiness after birth
If you end up not needing the colostrum after birth its still wonderful to have on hand for when your baby gets sick (hello amazing powerful antibodies!).
Top benefits of colostrum for babies:
High in immunoglobulins (IgA) to protect and coat the newborn gut
Supports gut closure, reducing permeability to pathogens
Stabilizes blood sugar (especially important for babies at risk of hypoglycemia)
Reduces inflammation
Easier to digest due to small volume and high nutrient density
Helps with meconium passage, reducing jaundice risk
Colostrum is biologically designed to match exactly what your newborn needs in those first hours and days.
Benefits of colostrum harvesting for parents:
Builds confidence with breast massage + hand expression
Encourages oxytocin release
Can help prepare tissue for early latch
Reduces stress during feeding challenges
Gives families a “backup plan” if baby needs supplementation
Helpful for people planning for NICU risk, gestational diabetes, or C-sections
When to Start Colostrum Harvesting Prenatally
Most families begin after 37 weeks when they have received medical clearance from their provider but keep reading for more specific details:
Typically recommended start times:
Low-risk pregnancies: 37–40 weeks
High-risk pregnancies: only when your provider approves
If planning for early delivery: your OB/MFM may recommend starting sooner
Expected collection timeline:
37–38 weeks: Drops, maybe up to 0.5–1 mL
38–39 weeks: Easier letdown, more familiarity might lead to more output
39–40 weeks: Some families may collect multiple mL per session
Every body is different. There is no “normal” amount and the amount that you collect prenatally is NOT associated with the amount of milk that you will make postpartum. If you are unable to express colostrum don't fret! Every time you try, you are becoming more confident in your hand expression skills and you are stimulating vital nerves in the breast that help create more milk ducts so keep trying!
When NOT to Hand Express Prenatally (Contraindications)
You should not start prenatal expression if you have:
History of preterm labor
Current contractions with nipple stimulation
Vasa previa, placenta previa, or bleeding
Shortened or unstable/incompetent cervix
High-risk pregnancy without clearance
Reduced fetal movement
Any condition your OB/MFM/Midwife advises against collection
Hand expression can stimulate oxytocin release, which may cause uterine tightening. Always check with your provider before starting hand expression/colostrum collection. Stop the collection process if you start to feel contractions while expressing.
What Supplies Do You Need for Safe Colostrum Collection?
You only need a few simple tools to safely collect colostrum:
Clean, sterile containers (at least one of the following):
1–5 mL sterile syringes with caps
Sterile collection cup
A spoon
Food-grade silicone colostrum collectors
Labels:
Sharpie + tape for syringes
Waterproof or erasable labels for larger containers that you plan to reuse
Clean environment:
Sanitize the surface you’ll use
Wash your hands and chest thoroughly
Warm, soothing environment:
Warmth encourages the milk ejection reflex (letdown), increases circulation, and softens breast tissue.
Try:
Warm compress or heating pad on your neck and shoulders
Warm shower preceding collection
Sitting in a warm (pregnancy safe) bath
An electronic breast warmer
Storage for on-the-go:
Ice packs
Insulated cooler
Step-by-Step: How to Hand Express Colostrum
Hand expression is often more effective than pumping for sticky early colostrum as its likely you will only get drops and if you are using a pump, these will get lost in the parts and you won't be able to store it. If you are someone who is able to collect an ounce or more in a short collection session, you may consider using a pump - but I still recommend using hand expression for some sessions in order to promote familiarity with the hand expression process.
1. Start with warmth and relaxation
Set yourself up with a relaxing environment. Use heat on your shoulders and neck for 1–5 minutes. While doing so, lower your stress (cortisol) levels by engaging in 10 deep, slow diaphragmatic breathes. Relax your shoulders, face, and jaw, and get comfortable.
2. Massage the breast
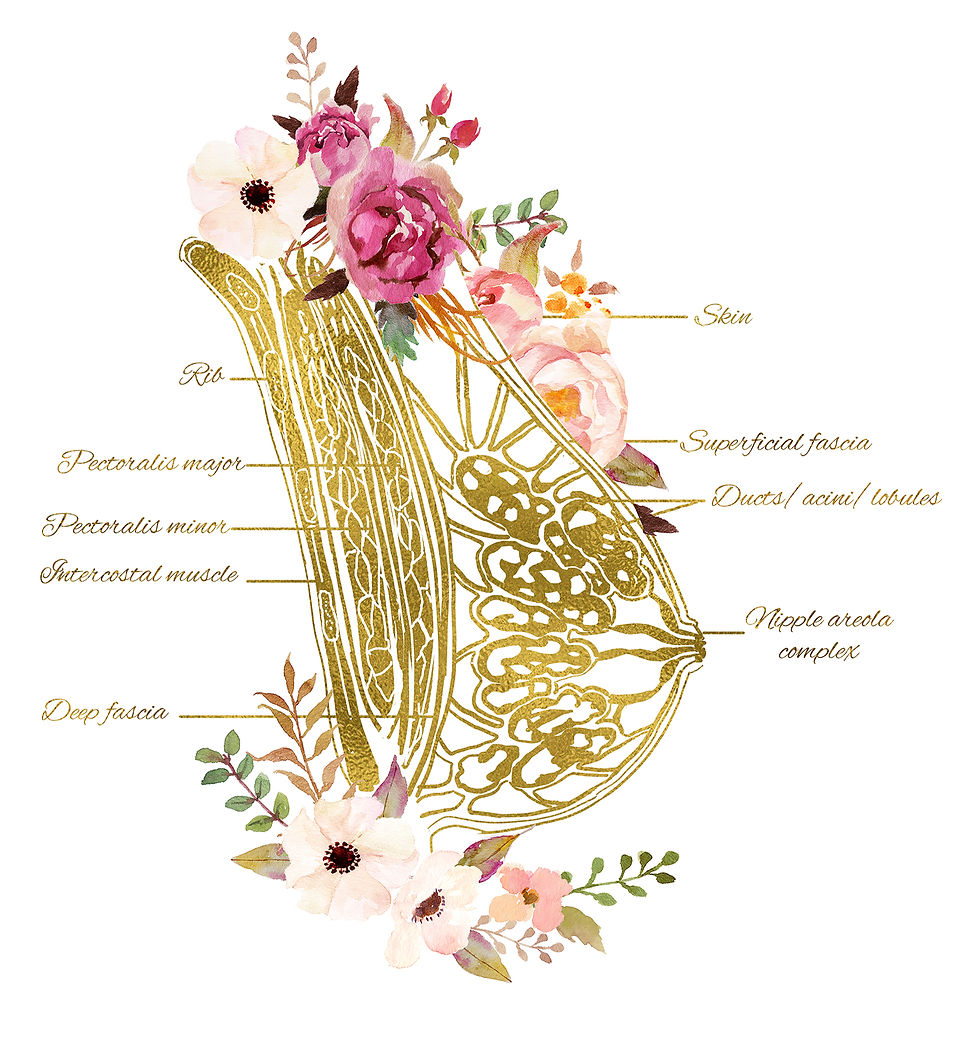
Use to fingers to complete gentle, circular motions over the whole breast - including the diagonal line from your nipple to your armpit area (yes—breast tissue is there too!). This helps stimulate blood flow to the breast tissue. It also helps "prime the pump" or release milk into the milk ducts from their storage cells (the alveoli - the peanut shaped cells in the image below), making it easier to express once you begin.
3. Form the C-hold
Using your hand on the same side as the breast, place your thumb on top of the breast and fingers underneath the areola on the opposite side of your thumb, about 1–1.5 inches behind the nipple.
4. Press back toward the chest
This positions your fingers behind the milk ducts.
5. Compress, roll, and release
In a gentle rhythmic motion, compress your fingers together slightly and roll the fingers forward until you reach the areola. You do not need to touch your nipple. Release, reset your fingers and repeat. Be sure to move slowly through this process. The number one mistake I see new expressers make is moving too quickly which does not allow enough time for the colostrum to move from the alveoli to the ducts.
Press back → compress → roll forward → release → repeat
6. Be patient with early drops
Typically colostrum will start as just small dots of colostrum on the nipple which gradually accumulate with each stroke. Because colostrum is so thick and sticky, it will typically remain on your nipple until the drop reaches a substantial size. Once this happens collect them by:
Touching the syringe to the droplet and applying suction
Gently scraping onto a spoon
Letting them drip into a sterile cup
If you are using the spoon or cup method, you can use the syringe/colostrum collector at the end of your session to suck up the liquid for storage.
7. Rotate around the breast
You have milk ducts and breast tissue surrounding your breast. Be sure to move your hand around the breast like rotating around a clock once you stop getting colostrum from one area.
8. Switch sides as needed
Follow your comfort—there’s no strict timing for this. If your wrist or fingers start getting tiered switch sides. While expressing, be sure to not over bend your wrist as this can cause carpal tunnel symptoms. Instead, aim to keep your wrist in neutral with your thumb in line with your forearm.
How Much Colostrum Should You Expect?
Completely normal amounts include:
Drops
0.2–1 mL
1–3 mL
Sometimes 10–30 mL
Output varies dramatically and does not predict future milk supply. Newborns only need milliliters per feed—not ounces—in the first 24–48 hours. In fact, on day 1 of life, most newborns will consume 5-7mL per feeding, which adds up to less than 2oz total their first 24 hours.
Pumping vs. Hand Expression: When to Use Each
Hand expression is best when:
Expressing prenatally
Collecting sticky early colostrum
You only get small drops
You want to stimulate oxytocin
A pump may help when:
You are collecting 30 mL or more
You had a complicated birth and its after the first 24-48 hours of hand expressing postpartum (hand expressing is better at stimulating more milk ducts to form - which sets you up for a better long-term milk supply)
Your provider requests additional stimulation
You’re 2+ days postpartum and transitioning to mature milk
You are absolutely too exhausted after birth to hand express every 2 hours. In this case, stimulation by the pump is better than nothing at all.
How to Store, Freeze, Thaw, and Transport Colostrum
Refrigerator:
Safe for 24 hours
Freezer (standard):
Up to 6 months (its best to store in the back of the freezer to prevent temperature changes from occurring when the freezer is opened throughout the day)
Deep freezer:
Up to 12 months
Thawing:
Hold the syringe in your warm hands rolling back and forth
Place it in your bra to defrost with your body heat
Run the center of the syringe under warm water
NEVER microwave
Transporting to the hospital:
Use ice packs and an insulated bag
Tell triage or labor nurses you’ve brought frozen colostrum
Ask that it be labeled and stored properly in the unit freezer
How to Feed Colostrum to Your Newborn
Depending on age, feeding ability, and medical needs, you may use:
Syringe feeding
Cup feeding
Spoon feeding
Finger feeding
Supplemental nursing system (SNS)
Direct breastfeeding
Typical intake in first 24 hours is only 5-7 mL per feed for 8-12 feeds per day. Their stomach is only the size of a marble!

Side note: These amounts are important to know if you hope to exclusively breastfeed. Take a picture of this image to reference later. Some hospitals may incorrectly recommend supplementation early. Always ask for a "weighted feed" before agreeing to supplementation if you hope to breastfeed exclusively.
Partner Support: How They Can Help
Partners can:
Prepare warm compresses
Help massage the upper back, shoulders, and feet
Hold the collection cup
Help label and freeze syringes
Offer encouragement during sessions
Bring snacks, water, and emotional support
Colostrum harvesting is a team activity!
Common Mistakes to Avoid
Pinching or pulling the nipple
Sliding fingers without compressing
Stressing about output
Skipping warmth
Not rotating around the breast
Comparing your output to others
Your body is doing it exactly right.
Trusted Video Demonstrations
These are the two videos I recommend to families because they are clear, accurate, and evidence-based:
Stanford Medicine Newborn Nursery — Hand Expression
Shows the C-hold, compress-release pattern, and how to collect early colostrum.
Global Health Media — “Hand Expressing the First Milk”
A gentle, parent-focused demonstration widely used in lactation education.
Need Personalized Support? I’m Here to Help.
If you’re in Eugene, Springfield, or the Lane County area, or want virtual lactation support from anywhere in the world, I’d love to help you:
🍼 Learn to hand express with confidence
👶 Support your baby’s feeding, tension, or tongue-tie
🌿 Prepare for a smoother breastfeeding journey
🤰 Get ready for birth with pelvic floor education
🌸 Thrive in the fourth trimester with expert guidance
Reach out anytime:
📸 @haliatherapeutics
📍 Serving families across the world
You deserve to feel supported, informed, and empowered.
And I’m here to walk that journey with you









Comments